Definition:
Septic endocarditis entities include acute, subacute bacterial endocarditis, previously called endocarditis lenta, as well as other non-bacterial endocarditis caused by a virus or fungus. The disease is a significant cause of morbidity and mortality in children, despite progress in treatment and prophylaxis.
Etiopathogenesis:
For the development of infective endocarditis in 50% of cases responsible Streptococcus viridans. In 30% of cases, with increasing frequency in recent decades, is responsible Staphylococcus pyogenes. The participation of other organisms is less common and 10% of blood cultures were negative.Staphylococcal endocarditis is less common in patients who have primary heart disease. Streptococcus (viridans) endocarditis occurs after dental surgery, and enterokokni (group D) after manipulation of the genitourinary tract and GIT. Pseudomonas aeruginosa occurs after IV drug use.
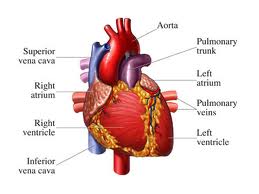
Endocarditis is the most common complication of congenital or rheumatic heart disease, but can also occur in those children who have no previous heart disease. The disease is extremely rare in the infant age. Vegetation is usually formed at the site of intimal or endocardial lesions are the result of turbulent blood flow high speed and thus, the greatest risk for the development of septic endocarditis having children with: VSD, valvular stenosis, especially the aorta, tetralogy of Fallot, patent ductus arteriosus, transposition of the great right vascular and surgical systemic-pulmonary shunts. In adults, this can add up bikuspidalna aortic valve, mitral valve prolapse with mitral regurgitation, the artificial valve.Surgical correction of heart disease reduces but does not eliminate the risk of endocarditis, except repair 6 months after ASD closure and DAP. Increased risk of developing this disease are drug users, and those who have a long-term presence of catheters in large veins by permanent perfusion or parenteral nutrition. Vegetation consisting of necrotic tissue, fibrin, which includes bacteria, white blood cells and calcifications. Necrotic tissue is easily crush creating septic emboli that may obstruct blood vessels both in the myocardium and in other areas of pulmonary and systemic circulation.
Clinical picture:
If the causative agent is Streptococcus viridans, the symptoms are generally mild with temperatures as prolonged loss of weight which may persist for several months. Contrary to this, the start can be very hectic with intermittent high fever, chills, fatigue, myalgia, arthralgia, headache, nausea, and vomiting.Objectively present the clinical findings of changes in the heart, changed the character's heartbeat, ekstratonova phenomenon, changing the character of noise or its appearance when it was not there before, and signs of congestive heart failure. Usually dominated by signs of mitral and aortic regurgitation. Splenomegaly was evident, and sometimes petechiae were present.
Neurological complications: embolism, cerebral abscesses, mikotične aneurysm and hemorrhage, manifested by signs of increased intracranial pressure, impaired senzorija tokalnim and neurological signs. Can be expected signs of systemic and pulmonary embolism.
Skin manifestations develop later in the disease, and are rarely seen in patients treated properly. These events are:
• Osler nodes (soft intradermal nodules on the side of your thumb palmarnoj)
• Janeway lesions (small erythematous or hemorrhagic painful lesions on the palms or soles)
• Splinter hemorrhages (linear lesions root of the nail)
• These lesions are probably caused by vasculitis, circulating antigen-antibody complexes.
Diagnosis:
The most important information to get the proper treatment haemoculture. Other laboratory data are of secondary importance are:
• Leukocytosis
• Hemolytic anemia
• rapidly
• microhematuria (a manifestation of immune complexes induced glomerulonephritis).
Blood culture done as soon as possible and in 3-5 times. In the first two blood cultures revealed the etiologic agent in 90% of cases. Previous antibacterial treatment to reduce blood culture positivity of 50-60%. Time sampling is not important since the expected constant bacteremia.
Echocardiography can reveal vegetation, identify their size, shape, location, and mobility as well as to determine the presence of valvular dysfunction. You can help in predicting complications emboličkih as lesions greater than 1 cm have a higher risk of embolization.
Prognosis and complications:
Forecast septic endocarditis is still serious. The mortality rate is 20-25%, and complications can be expected in 50-60% of children with documented disease.
The most common complications are:
• Congestive heart failure
• myocardial abscesses
• toxic myocarditis
• systemic embolization with signs of the CNS
• pulmonary embolism
• mikotične aneurysm
• ruptured sinus Valsalva
• acquired VSD
• disruptions in the implementation of pulse
Treatment:
Antibiotic treatment should be applied immediately after the diagnosis. A little delay could give progressive endocarditis with severe complications. One must keep a high level of bactericidal antibiotics long enough to eradicira microorganism that settled on the relatively avascular vegetation.Recommended duration of treatment within 4 to 6 weeks. The choice of antibiotics on the etiologic agent.
If it comes to Streptococcus viridans which is well susceptible to penicillin, then penicillin G is given in millions of doses, 200000-300000 IU / kg / day in 6 divided doses (every 4 hours), but not to exceed 20,000,000 for 24 hours . Alternatively given penicillin G plus gentaimicina iv 2-4 mg / kg / day in 3 divided doses, but not to exceed 80 mg / day.
If the cause of enterokokus which is less susceptible to penicillin, the preferred combination of iv Ampicillin 300 mg / kg / day in 4 divided doses with those that do not exceed 12 g / day, and gentamicin in the mentioned dose.
If the causative agent is Staphylococcus then semisintetski penicillins - oxacillin 200 mg / kg / day iv in 4 divided doses, but not to exceed 12 g / day.
Depending on the clinical response to therapy, in some cases it is necessary to prolong the treatment, and the highly sensitive infection with Streptococcus viridans may be recommended to shorten treatment time and include oral administration. If the heart is brought into a state of refractory congestive need the surgery, when the incorporation of artificial life-saving valve. Surgical replacement of the infected artificial valve has a large operational risk.
Prevention of septic endocarditis:
Surgical, dental procedures and the use of numerous instruments from different diagnostic and therapeutic procedures of mucosal damage caused by contamination of tissues with transient bacteremia that rarely persists for more than 15 minutes. These pathogens can settle on damaged, abnormal heart valves or heart defects in causing bacterial endocarditis or endarteritis.
Prophylactic use of antibiotics is recommended for patients who are at risk for developing endocarditis and underwent surgery that can cause bacteriemia. To avoid resistance to antibiotics used, prophylaxis is only used during the perioperative periods. 1 to 2 hours before surgery and 6 to 8 hours after.
State at risk for developing bacterial endocarditis:
• built-in artificial heart valves including bioprostetičke and homograft valves
• previous bacterial endocarditis, even in the absence of heart disease
• The majority of congenital cardiac malformations
• rheumatic valvular dysfunction or other etiology even after surgical intervention urađenog
• Hypertrophic Cardiomyopathy
• mitral valve prolapse with mitral regurgitation
Procedures that may cause bacteriemia:
• The majority of surgical procedures
• dental procedures that are known to cause gingival bleeding or mucous
Some conditions that are very close to the state where there is a risk of bacterial endocarditis but still bacterial endocarditis prophylaxis is not recommended:
• isolated ASD type sec.
• state after surgical correction without residue to 6 months after ASD correction type sec., VSD and patent ductus arteriosus
• mitral valve prolapse without mitral regurgitation - physiological, functional or inocentni noise
• previous Kawasaki-eva and rheumatic disease without valvular dysfunction
Some procedures that are close to those that can cause bacteriemia but still bacterial endocarditis prophylaxis is not recommended:
• stopping teeth chewing over the line
• Setting ortodontalnih appliances
• intraoral injections of anesthesia
• loss of primary teeth
• sectio caesarea
• uncomplicated vaginal delivery
The most numerous procedures that can cause bacteriemia smatotologije in the area. Poor oral hygiene, periodontal and periapical infections can cause bacteriemia even in the absence of dental procedures.People who have a risk of developing bacterial endocarditis should have the best possible oral health to eliminate a potential source of bakteriemije. Dentists should be reduced for patients with gingival inflammation stimulate brushing, rinsing with dezifencionim resources and professional teeth cleaning prior to performing routine dental procedures.
Before tooth extraction for 3 to 5 minutes to dry gum should be coated with CHLOREXIDINOM or povidone-iodine with because it has been proven that reduvira postekstrakcionu bacteriemia. If there is a dental procedure in the series then it is recommended to perform a seven-day intervals to reduce the potential risk of developing drug-resistant microorganisms, and patients without teeth may have the potential risk of ulceration due to bakteriemije mucosa that result from inadequately furnished prosthesis.
The most common cause of endocarditis following dental and surgical procedures in the upper respiratory tract (tonsils and / or adenoidectomy) is an α-hemolytic streptococcus and specific prophylaxis should be directed to the agent.
For a standard prophylactic regimen for all dental, oral surgical and surgical procedures in the upper respiratory tract is recommended amoxicillin. Amoxicillin is preferred over ampicillin and penicillin V due to its better absorption in the Gita, and the higher and more permanent level in the blood.
Granted to:
• AMOXICILLIN 50 mg / kg orally 1h before surgery, 25 mg / kg orally 6 to 8 hours after the initial dose. Being allergic to Amoxicillin / Penicillin or erythromycin given clyndamycin
• Erythromycin 20 mg / kg orally 2 h before surgery, 10 mg / kg orally 6 to 8 hours after the initial dose alternative
• CLYNDAMYCIN 10 mg / kg orally 1 hour before surgery, 5 mg / kg orally 6 to 8 hours after the initial dose. Total pediatric dose may exceed adult dose.
To determine the initial pediatric dose of amoxicillin can use the following scheme:
• below 15 kg body weight 750 mg amoxicillin
• 15 to 30 kg 1500 mg
• over 30 kg 3000 mg (adult dose)
• Doses below 1/2 of the initial dose.
Individuals who are unable to take medication orally recommended parenteral ampicillin.
Ampicillin 50 mg / kg im or iv 30 minutes before the procedure 25 mg / kg / m. or iv 6 hours after the initial dose. Being allergic to Ampicillin / Penicillin given Clyndamycin.
CLYNDAMYCIN 10 mg / kg iv 30 minutes prior to the procedure 5 mg / kg iv 6 hours after the initial dose.
Very high risk of developing endocarditis are those with artificial valves, surgically constructed systemic-pulmonary Santo, conduit and persons who have a history of earlier data prebolovanom endocarditis. In such persons develop endocarditis is associated with high mortality. In such persons recommended the combination of ampicillin and parenteral Gentamycin.
• Ampicillin 50 mg / kg im or iv 30 min. before surgery
• Gentamicin 2 mg / kg im or iv 30 min. before the procedure (not to exceed 80 mg). After 8 hours of repeating the initial dose regimen in full. Being allergic to Ampicillin / Penicillin given vancomycin.
• VANCOMYCIN 20 mg / kg iv perfusion for a period of 1 hour (to start 1 hour prior to surgery)
• Repeat dose is not necessary.
Bakteriemija can develop in surgical procedures and the use of different instruments for diagnostic and therapeutic purposes in genito-urinary and gastrointestinal tract. Bacterial endocarditis arising after such surgery usually is caused by Enterococcus foecalis. Antibiotic prophylaxis should be tailored to the agent. These requirements will meet the combination of:
• Ampicillin and Gentamycin as indicated above.
• If you are allergic to Ampicillin / Penicillin given combination VANCOMYCIN and Gentamycin.
• If you are low-risk patients in this group of patients is sufficient AMOXICILLIN orally.
• Tetracyclines and sulfonamides are not recommended in the prophylaxis of endocarditis.